This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (CC BY).
ORIGINAL RESEARCH
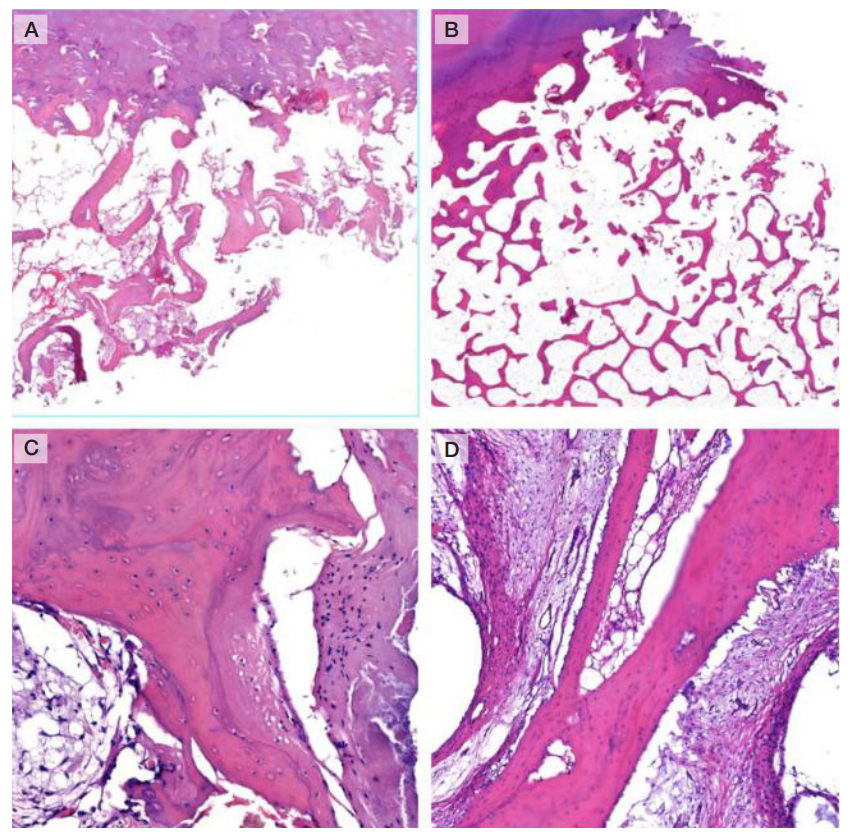
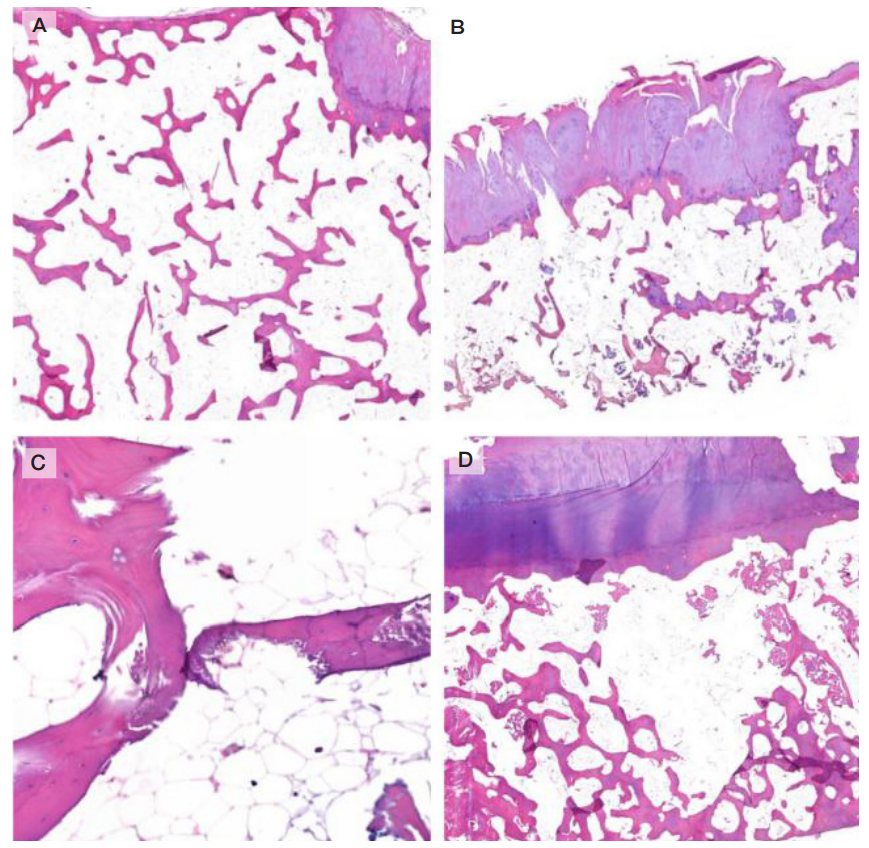
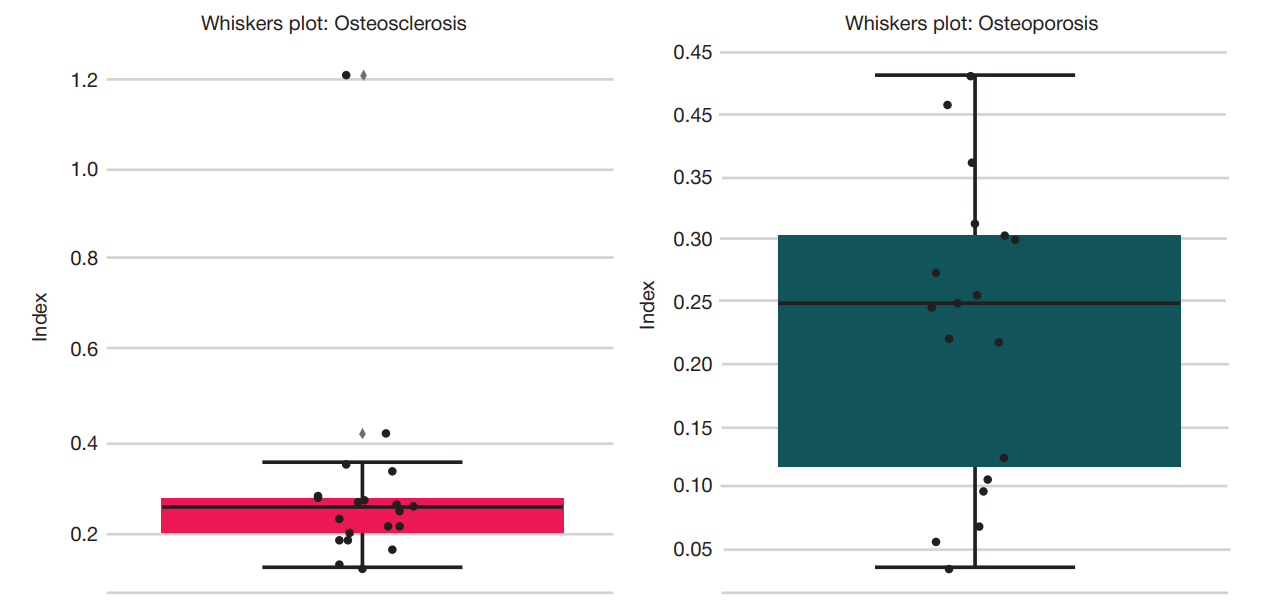
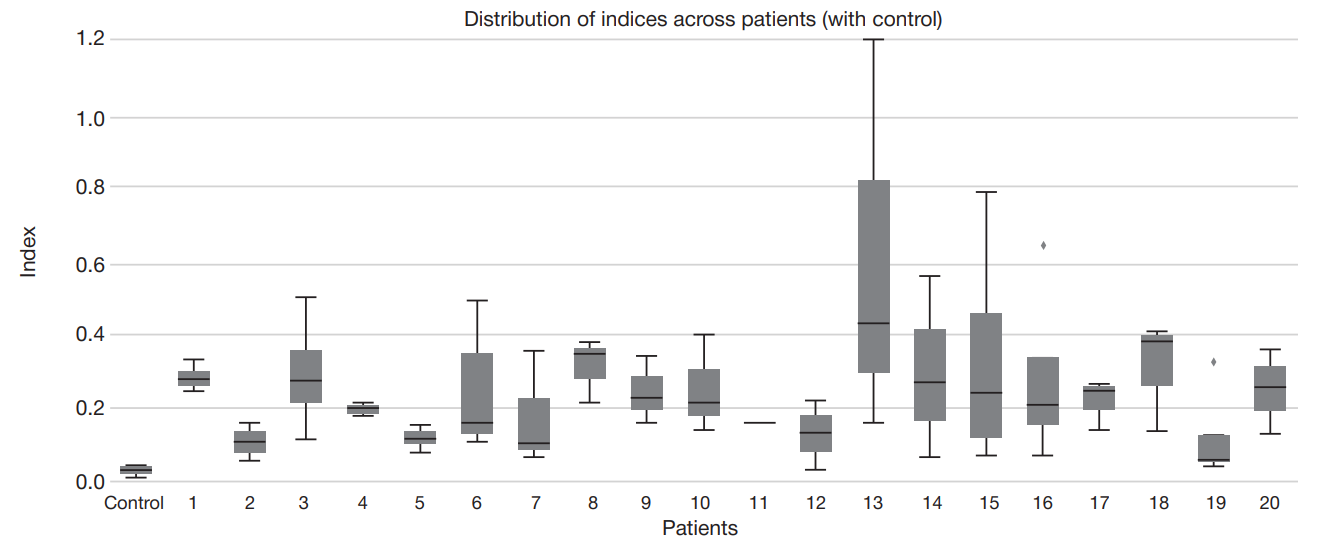
Morphological subchondral bone tissue characteristics in knee osteoarthritis
1 Bashkir State Medical University, Ufa, Russia
2 Avicenna Tajik State Medical University, Dushanbe, Tajikistan
Correspondence should be addressed: Vladislav N. Akbashev
Lenina, 3, Ufa, 450008, Russia; ur.liam@bka-dalv
Author contribution: Minasov BSh — study concept and design, data analysis and interpretation, manuscript editing; Yakupov RR — material collection, morphological assessment, primary data processing; Akbashev VN — statistical processing, visualization of results, manuscript writing; Shchekin VS — literature review, morphology data interpretation; Vlasova AO — preparing illustrations, morphometry analysis, manuscript proofreading; Minasov TB — preparing illustrations, discussion; Karimov KK — material collection, clinical follow-up of patients; Akhmeldinova AA — drawing up inclusion/exclusion criteria, coordination of ethical approval.
Compliance with ethical standards: the study was approved by the Ethics Committee of the Bashkir State Medical University (protocol No. 3 dated 12 March 2025) and conducted in accordance with the World Medical Association Declaration of Helsinki (2013 revision). All patients submitted the informed consent to participation in the study.